Introduction: Pain secondary to vaso-occlusive episodes (VOE) is one of the most common and debilitating complications of sickle cell disease (SCD). Although there are guidelines for pain management, these are often not well-followed. Pain management is entrenched in subjectivity and susceptible to implicit bias. Research has shown that clinical pathways improve care for patients which is especially important in vulnerable populations such as pediatric patients with SCD. Following a quality improvement project at our institution that resulted in significantly improved inpatient care for pediatric patients with SCD, the goal of this project was to create an accessible clinical pathway with multidisciplinary input to streamline management of VOE in the emergency department (ED) and assure equitable care for all. We aimed to improve time to analgesics, increase the percent of patients receiving pain medications within 30 minutes, and increase intranasal fentanyl and patient-controlled anesthesia (PCA) utilization in the pediatric ED.
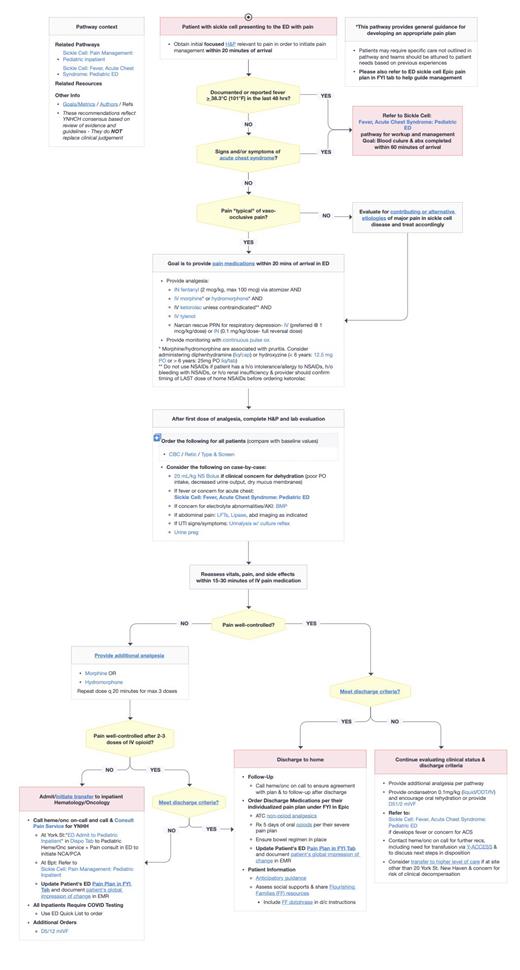
Methods: The care signature clinical pathway was created using a multidisciplinary approach with individuals representing the department of pediatric hematology-oncology, pediatric emergency, anesthesiology, pharmacy, and nurse management. The pathway was developed based on updated American Society of Hematology guidelines for pain management in pediatric VOE. The pathway became available for use via electronic medical record on July 12 th, 2022. Outcome measures regarding pain management were evaluated for one year prior to pathway publication and compared to outcomes one year after publication. Patients with a primary or secondary diagnosis of SCD presenting to the Yale pediatric ED with vaso-occlusive pain were included.
Results: A total of 214 ED visits were evaluated. The pre-pathway cohort included 108 encounters from July 1 st, 2021 to June 30 th, 2022 and the post-pathway cohort included 106 ED encounters from August 1 st, 2022 to July 21 st, 2023. During the first year post implementation, a provider utilized the clinical pathway a total of 534 times (121 individuals) with an average of 1 time per day. An analgesic was ordered for 63 (58.3%) patients and administered for 31 (28.7%) patients within 30 minutes of arrival in the pre-pathway cohort. An analgesic was ordered for 73 (68.9%) and administered for 32 (30.2%) patients within 30 minutes of arrival in the post-pathway cohort. Comparing pre- and post-pathway cohorts, the median time to pain medication order was 22 vs 17 minutes and pain medication administration was 42 vs 40 minutes respectively. Intranasal fentanyl was used for 2 (1.9%) patients in the pre-pathway cohort and 12 (11.3%) patients in the post-pathway cohort. A total of 0 (0%) hydromorphone PCAs were administered in the ED in the pre-pathway cohort compared to 4 (3.8%) hydromorphone PCA administered in the ED in the post-pathway cohort.
Conclusion: Standardizing pain management using a clinical pathway has shown improvement in ED management of VOE in the first year post implementation with increased utilization of intranasal fentanyl and PCAs. Our goal of increased percentage of patients receiving pain medication within 30 minutes and decreased time to first analgesic was not achieved, however this is an ongoing project and with education in implementation of the clinical pathway we hope to continue to see long term progress. Additionally, in the future, we plan to expand use of this pathway to additional sites within our health care system.
Disclosures
No relevant conflicts of interest to declare.